Antimicrobial resistance

Antibiotic resistance tests: Bacteria are streaked on dishes with white disks, each impregnated with a different antibiotic. Clear rings, such as those on the left, show that bacteria have not grown—indicating that these bacteria are not resistant. The bacteria on the right are fully susceptible to only three of the seven antibiotics tested.[1]
Antimicrobial resistance (AMR or AR) is the ability of a microbe to resist the effects of medication that once could successfully treat the microbe.[2][3][4] The term antibiotic resistance (AR or ABR) is a subset of AMR, as it applies only to bacteria becoming resistant to antibiotics.[3] Resistant microbes are more difficult to treat, requiring alternative medications or higher doses of antimicrobials. These approaches may be more expensive, more toxic or both. Microbes resistant to multiple antimicrobials are called multidrug resistant (MDR). Those considered extensively drug resistant (XDR) or totally drug resistant (TDR) are sometimes called "superbugs".[5]
Resistance arises through one of three mechanisms: natural resistance in certain types of bacteria, genetic mutation, or by one species acquiring resistance from another.[6] All classes of microbes can develop resistance. Fungi develop antifungal resistance. Viruses develop antiviral resistance. Protozoa develop antiprotozoal resistance, and bacteria develop antibiotic resistance. Resistance can appear spontaneously because of random mutations. However, extended use of antimicrobials appears to encourage selection for mutations which can render antimicrobials ineffective.[7]
Preventive measures include only using antibiotics when needed, thereby stopping misuse of antibiotics or antimicrobials.[8][9] Narrow-spectrum antibiotics are preferred over broad-spectrum antibiotics when possible, as effectively and accurately targeting specific organisms is less likely to cause resistance.[10] For people who take these medications at home, education about proper use is essential. Health care providers can minimize spread of resistant infections by use of proper sanitation and hygiene, including handwashing and disinfecting between patients, and should encourage the same of the patient, visitors, and family members.[11]
Rising drug resistance is caused mainly by use of antimicrobials in humans and other animals, and spread of resistant strains between the two.[8] Growing resistance has also been linked to dumping of inadequately treated effluents from the pharmaceutical industry, especially in countries where bulk drugs are manufactured.[12] Antibiotics increase selective pressure in bacterial populations, causing vulnerable bacteria to die; this increases the percentage of resistant bacteria which continue growing. Even at very low levels of antibiotic, resistant bacteria can have a growth advantage and grow faster than vulnerable bacteria.[13] With resistance to antibiotics becoming more common there is greater need for alternative treatments. Calls for new antibiotic therapies have been issued, but new drug development is becoming rarer.[14]
Antimicrobial resistance is increasing globally because of greater access to antibiotic drugs in developing countries.[15] Estimates are that 700,000 to several million deaths result per year.[16][17] Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die as a result.[18] There are public calls for global collective action to address the threat that include proposals for international treaties on antimicrobial resistance.[19] Worldwide antibiotic resistance is not completely identified, but poorer countries with weaker healthcare systems are more affected.[9]
.mw-parser-output .toclimit-2 .toclevel-1 ul,.mw-parser-output .toclimit-3 .toclevel-2 ul,.mw-parser-output .toclimit-4 .toclevel-3 ul,.mw-parser-output .toclimit-5 .toclevel-4 ul,.mw-parser-output .toclimit-6 .toclevel-5 ul,.mw-parser-output .toclimit-7 .toclevel-6 ul{display:none}
Contents
1 Definition
2 Overview
3 Causes
3.1 Clinical significance
3.2 Veterinary medicine
3.3 Natural occurrence
3.4 Water pollution
4 Prevention
4.1 Duration of antibiotics
4.2 Monitoring and mapping
4.3 Limiting antibiotic use
4.3.1 At the hospital level
4.3.2 At the level of GP
4.3.3 At the individual level
4.3.4 Country examples
4.4 Water, sanitation, hygiene
4.5 Industrial wastewater treatment
4.6 Management in animal use
4.6.1 Europe
4.6.2 United States
4.7 Global action plans and awareness
4.7.1 Antibiotic Awareness Week
5 Mechanisms and organisms
5.1 Fundamentals
5.2 Bacteria
5.3 Viruses
5.4 Fungi
5.5 Parasites
6 History
7 Society and culture
7.1 Legal frameworks
7.1.1 U.S.
7.2 Policies
8 Further research
8.1 Vaccines
8.2 Alternating therapy
8.3 Development of new drugs
8.4 Rapid diagnostics
8.5 Phage therapy
9 See also
10 References
10.1 Books
10.2 Journals
11 External links
Definition
Diagram showing the difference between non-resistant bacteria and drug resistant bacteria. Non-resistant bacteria multiply, and upon drug treatment, the bacteria die. Drug resistant bacteria multiply as well, but upon drug treatment, the bacteria continue to spread.[20]
The WHO defines antimicrobial resistance as a microorganism's resistance to an antimicrobial drug that was once able to treat an infection by that microorganism.[3]
A person cannot become resistant to antibiotics. Resistance is a property of the microbe, not a person or other organism infected by a microbe.[21]
Overview
A World Health Organization (WHO) report released April 2014 stated, "this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country. Antibiotic resistance—when bacteria change so antibiotics no longer work in people who need them to treat infections—is now a major threat to public health."[22] The European Centre for Disease Prevention and Control calculated that in 2015 there were 671,689 infections in the EU and European Economic Area caused by antibiotic-resistant bacteria, resulting in 33,110 deaths. Most were acquired in healthcare settings.[23]
Causes

How antibiotic resistance evolves and spreads
Bacteria with resistance to antibiotics predate medical use of antibiotics by humans.[24][25] However, widespread antibiotic use has made more bacteria resistant through the process of evolutionary pressure.[26][7]
Reasons for the widespread use of antibiotics in human medicine include:
- increasing global availability over time since the 1950s
- uncontrolled sale in many low or middle income countries, where they can be obtained over the counter without a prescription, potentially resulting in antibiotics being used when not indicated.[27]:1060 This may result in emergence of resistance in any remaining bacteria.
Other causes include:
Antibiotic use in livestock feed at low doses for growth promotion is an accepted practice in many industrialized countries and is known to lead to increased levels of resistance.[28][29]
- Releasing large quantities of antibiotics into the environment during pharmaceutical manufacturing through inadequate wastewater treatment increases the risk that antibiotic-resistant strains will develop and spread.[30][31]
- It is uncertain whether antibacterials in soaps and other products contribute to antibiotic resistance, but antibacterial soaps are discouraged for other reasons.[32][33]
Antiseptics create AMR to antibiotics and other antiseptics:
Antiseptics appear to activate tolerance mechanisms in bacteria, which offer them protection against a range of antiseptics as well as antibiotics. Antiseptics are used for cleaning in hospitals and in many wound care dressings. These findings may explain the increase in treatment-resistant hospital infections.
Exposure to low doses of the antiseptic octenidine allowed several different strains of Pseudomonas aeruginosa to develop cross-tolerance to other antiseptics and to several different antibiotics.[34] The level of tolerance was substantial, i.e. in several cases a 32-fold increase in concentrations of the antiseptic was required to obtain the same antimicrobial effect. Also, this increased resistance was permanent. The same group also reported[35] that Klebsiella pneumoniae was able to develop tolerance to chlorhexidine and that 5 out of 6 strains showed cross-resistance to the last-resort antibiotic, colistin.
Clinical significance
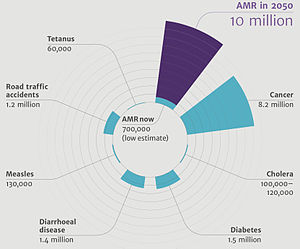
Deaths attributable to antimicrobial resistance every year compared to other major causes of death.[17]
Increasing bacterial resistance is linked with the volume of antibiotic prescribed, as well as missing doses when taking antibiotics.[36] Inappropriate prescribing of antibiotics has been attributed to a number of causes, such as patients insisting on antibiotics and physicians prescribing them as they do not have time to explain why they are not necessary. Another cause can be physicians not knowing when to prescribe antibiotics or being overly cautious for medical or legal reasons.[37] For example, 70 to 80 percent of diarrhea is caused by viral pathogens, for which antibiotics are not effective. But nevertheless, around 40 percent of these cases are attempted to be treated with antibiotics.[38] In some areas even over 80 percent of such cases are attempted to be treated with antibiotics.[38]
Lower antibiotic concentration contributes to the increase of AMR by introducing more mutations that support bacterial growth in higher antibiotic concentration. For example, sub-inhibitory concentration have induced genetic mutation in bacteria such as Pseudomonas aeruginosa and Bacteroides fragilis.[39]
Up to half of antibiotics used in humans are unnecessary and inappropriate.[8] For example, a third of people believe that antibiotics are effective for the common cold,[40] and the common cold is the most common reason antibiotics are prescribed even though antibiotics are useless against viruses.[41] A single regimen of antibiotics even in compliant individuals leads to a greater risk of resistant organisms to that antibiotic in the person for a month to possibly a year.[42][43]
Antibiotic resistance increases with duration of treatment. Therefore, as long as an effective minimum is kept, shorter courses of antibiotics are likely to decrease rates of resistance, reduce cost, and have better outcomes with fewer complications.[10] Short course regimens exist for community-acquired pneumonia[44]spontaneous bacterial peritonitis,[45] suspected lung infections in intense care wards,[46] so-called acute abdomen,[47] middle ear infections, sinusitis and throat infections,[48] and penetrating gut injuries.[49][50] In some situations a short course may not cure the infection as well as a long course.[51] A BMJ editorial recommended that antibiotics can often be safely stopped 72 hours after symptoms resolve.[52]
Because individuals may feel better before the infection is eradicated, doctors must provide instructions to them so they know when it is safe to stop taking a prescription. Some researchers advocate doctors' using a very short course of antibiotics, reevaluating the patient after a few days, and stopping treatment if there are no clinical signs of infection.[53]
Certain antibiotic classes result in resistance more than others. Increased rates of MRSA infections are seen when using glycopeptides, cephalosporins, and quinolone antibiotics.[54][55] Cephalosporins, and particularly quinolones and clindamycin, are more likely to produce colonisation with Clostridium difficile.[56][57]
Factors within the intensive care unit setting such as mechanical ventilation and multiple underlying diseases also appear to contribute to bacterial resistance.[58] Poor hand hygiene by hospital staff has been associated with the spread of resistant organisms.[59]
Counterfeit medications may contain sub-therapeutic concentrations of antibiotics, designed to reduce the chance of detection, and this by definition, increases antimicrobial resistance.[60]
Veterinary medicine

All animals carry bacteria in their intestines. Antibiotics are given to animals. Antibiotics kill most bacteria. But resistant bacteria survive and multiply.
The World Health Organization concluded that inappropriate use of antibiotics in animal husbandry is an underlying contributor to the emergence and spread of antibiotic-resistant germs, and that the use of antibiotics as growth promoters in animal feeds should be restricted.[61] The World Organisation for Animal Health has added to the Terrestrial Animal Health Code a series of guidelines with recommendations to its members for the creation and harmonization of national antimicrobial resistance surveillance and monitoring programs,[62] monitoring of the quantities of antibiotics used in animal husbandry,[63] and recommendations to ensure the proper and prudent use of antibiotic substances. Another guideline is to implement methodologies that help to establish associated risk factors and assess the risk of antibiotic resistance.[64]
Natural occurrence
Naturally occurring antibiotic resistance is common.[65] Genes for resistance to antibiotics, like antibiotics themselves, are ancient.[66][67] The genes that confer resistance are known as the environmental resistome.[65] These genes may be transferred from non-disease-causing bacteria to those that do cause disease, leading to clinically significant antibiotic resistance.[65]
In 1952 it was shown that penicillin-resistant bacteria existed before penicillin treatment;[68] and also preexistent bacterial resistance to streptomycin.[69] In 1962, the presence of penicillinase was detected in dormant endospores of Bacillus licheniformis, revived from dried soil on the roots of plants, preserved since 1689 in the British Museum.[70][71][72] Six strains of Clostridium, found in the bowels of William Braine and John Hartnell (members of the Franklin Expedition) showed resistance to cefoxitin and clindamycin.[73]
Penicillinase may have emerged as a defense mechanism for bacteria in their habitats, such as the case of penicillinase-rich Staphylococcus aureus, living with penicillin-producing Trichophyton; however, this may be circumstantial.[72] Search for a penicillinase ancestor has focused on the class of proteins that must be a priori capable of specific combination with penicillin.[74] The resistance to cefoxitin and clindamycin in turn was attributed to Braine's and Hartnell's contact with microorganisms that naturally produce them or random mutation in the chromosomes of Clostridium strains.[73]
There is evidence that heavy metals and other pollutants may select for antibiotic-resistant bacteria, generating a constant source of them in small numbers.[75]
Water pollution
Antibiotic resistance is a growing problem among humans and wildlife in terrestrial or aquatic environments. In this respect, the spread and contamination of the environment, especially through water pollution "hot spots" such as hospital wastewater and untreated urban wastewater, is a growing and serious public health problem.[76][77] Antibiotics have been polluting the environment since their introduction through human waste (medication, farming), animals, and the pharmaceutical industry.[78] The contribution of the pharmaceutical industry is so significant that parallels can be drawn between countries with highest rate of increasing antibiotic resistance and countries with largest footprint of pharmaceutical industry. China, which contributes to nearly 90 per cent of the world's active pharmaceutical ingredient (API) manufacturing, has seen a 22 per cent increase in rate of antimicrobial resistance in six years, compared to a 6 per cent increase in the United States.[79]
Along with antibiotic waste, resistant bacteria follow, thus introducing antibiotic-resistant bacteria into the environment. Already in 2011, mapping of sewage and water supply samples in New Delhi showed widespread and uncontrolled infection as indicated by the presence of NDM-1-positive enteric bacteria (New Delhi metallo-beta-lactamase 1).[80]
As bacteria replicate quickly, the resistant bacteria that enter water bodies through wastewater replicate their resistance genes as they continue to divide. In addition, bacteria carrying resistance genes have the ability to spread those genes to other species via horizontal gene transfer. Therefore, even if the specific antibiotic is no longer introduced into the environment, antibiotic-resistance genes will persist through the bacteria that have since replicated without continuous exposure.[78] Antibiotic resistance is widespread in marine vertebrates, and they may be important reservoirs of antibiotic-resistant bacteria in the marine environment.[81]
Prevention

Mission Critical: Preventing Antibiotic Resistance (CDC report, 2014)
There have been increasing public calls for global collective action to address the threat, including a proposal for international treaty on antimicrobial resistance. Further detail and attention is still needed in order to recognize and measure trends in resistance on the international level; the idea of a global tracking system has been suggested but implementation has yet to occur. A system of this nature would provide insight to areas of high resistance as well as information necessary for evaluation of programs and other changes made to fight or reverse antibiotic resistance.
Duration of antibiotics
Antibiotic treatment duration should be based on the infection and other health problems a person may have.[10] For many infections once a person has improved there is little evidence that stopping treatment causes more resistance.[10] Some therefore feel that stopping early may be reasonable in some cases.[10] Other infections, however, do require long courses regardless of whether a person feels better.[10]
Monitoring and mapping
There are multiple national and international monitoring programs for drug-resistant threats, including methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant S. aureus (VRSA), extended spectrum beta-lactamase (ESBL), vancomycin-resistant Enterococcus (VRE), multidrug-resistant A. baumannii (MRAB).[82]
ResistanceOpen is an online global map of antimicrobial resistance developed by HealthMap which displays aggregated data on antimicrobial resistance from publicly available and user submitted data.[83][84] The website can display data for a 25-mile radius from a location. Users may submit data from antibiograms for individual hospitals or laboratories. European data is from the EARS-Net (European Antimicrobial Resistance Surveillance Network), part of the ECDC.
ResistanceMap is a website by the Center for Disease Dynamics, Economics & Policy and provides data on antimicrobial resistance on a global level.[85]
Limiting antibiotic use
Antibiotic stewardship programmes appear useful in reducing rates of antibiotic resistance.[86]
Excessive antibiotic use has become one of the top contributors to the development of antibiotic resistance. Since the beginning of the antibiotic era, antibiotics have been used to treat a wide range of disease.[87] Overuse of antibiotics has become the primary cause of rising levels of antibiotic resistance. The main problem is that doctors are willing to prescribe antibiotics to ill-informed individuals who believe that antibiotics can cure nearly all illnesses, including viral infections like the common cold. In an analysis of drug prescriptions, 36% of individuals with a cold or an upper respiratory infection (both viral in origin) were given prescriptions for antibiotics.[88] These prescriptions accomplished nothing other than increasing the risk of further evolution of antibiotic resistant bacteria.
At the hospital level
Antimicrobial stewardship teams in hospitals are encouraging optimal use of antimicrobials.[89] The goals of antimicrobial stewardship are to help practitioners pick the right drug at the right dose and duration of therapy while preventing misuse and minimizing the development of resistance. Stewardship may reduce the length of stay by an average of slightly over 1 day while not increasing the risk of death.[90]
At the level of GP
Given the volume of care provided in primary care (General Practice), recent strategies have focused on reducing unnecessary antibiotic prescribing in this setting. Simple interventions, such as written information explaining the futility of antibiotics for common infections such as upper respiratory tract infections, have been shown to reduce antibiotic prescribing.[91]
The prescriber should closely adhere to the five rights of drug administration: the right patient, the right drug, the right dose, the right route, and the right time.[92]
Cultures should be taken before treatment when indicated and treatment potentially changed based on the susceptibility report.[11][93]
About a third of antibiotic prescriptions written in outpatient settings in the United States were not appropriate in 2010 and 2011. Doctors in the U.S. wrote 506 annual antibiotic scripts for every 1,000 people, with 353 being medically necessary.[94]
Health workers and pharmacists can help tackle resistance by: enhancing infection prevention and control; only prescribing and dispensing antibiotics when they are truly needed; prescribing and dispensing the right antibiotic(s) to treat the illness.[22]
At the individual level
People can help tackle resistance by using antibiotics only when prescribed by a doctor; completing the full prescription, even if they feel better; never sharing antibiotics with others or using leftover prescriptions.[22]
Country examples
- The Netherlands has the lowest rate of antibiotic prescribing in the OECD, at a rate of 11.4 defined daily doses (DDD) per 1,000 people per day in 2011.
Germany and Sweden also have lower prescribing rates, with Sweden's rate having been declining since 2007.
Greece, France and Belgium have high prescribing rates of more than 28 DDD.[95]
Water, sanitation, hygiene
Infectious disease control through improved water, sanitation and hygiene (WASH) infrastructure needs to be included in the antimicrobial resistance (AMR) agenda. The "Interagency Coordination Group on Antimicrobial Resistance" stated in 2018 that "the spread of pathogens through unsafe water results in a high burden of gastrointestinal disease, increasing even further the need for antibiotic treatment."[96] This is particularly a problem in developing countries where the spread of infectious diseases caused by inadequate WASH standards is a major driver of antibiotic demand.[38] Growing usage of antibiotics together with persistent infectious disease levels have led to a dangerous cycle in which reliance on antimicrobials increases while the efficacy of drugs diminishes.[38] The proper use of infrastructure for water, sanitation and hygiene (WASH) can result in a 47–72 percent decrease of diarrhea cases treated with antibiotics depending on the type of intervention and its effectiveness.[38] A reduction of the diarrhea disease burden through improved infrastructure would result in large decreases in the number of diarrhea cases treated with antibiotics. This was estimated as ranging from 5 million in Brazil to up to 590 million in India by the year 2030.[38] The strong link between increased consumption and resistance indicates that this will directly mitigate the accelerating spread of AMR.[38] Sanitation and water for all by 2030 is Goal Number 6 of the Sustainable Development Goals.
An increase in hand washing compliance by hospital staff results in decreased rates of resistant organisms.[97]
Water supply and sanitation infrastructure in health facilities offer significant co-benefits for combatting AMR, and investment should be increased.[96] There is much room for improvement: WHO and UNICEF estimated in 2015 that globally 38% of health facilities did not have a source of water, nearly 19% had no toilets and 35% had no water and soap or alcohol-based hand rub for handwashing.[98]
Industrial wastewater treatment
Manufacturers of antimicrobials need to improve the treatment of their wastewater (by using industrial wastewater treatment processes) to reduce the release of residues into the environment.[96]
Management in animal use
Europe
In 1997, European Union health ministers voted to ban avoparcin and four additional antibiotics used to promote animal growth in 1999.[99] In 2006 a ban on the use of antibiotics in European feed, with the exception of two antibiotics in poultry feeds, became effective.[100] In Scandinavia, there is evidence that the ban has led to a lower prevalence of antibiotic resistance in (nonhazardous) animal bacterial populations.[101] As of 2004, several European countries established a decline of antimicrobial resistance in humans through limiting the usage antimicrobials in agriculture and food industries without jeopardizing animal health or economic cost.[102]
United States
The United States Department of Agriculture (USDA) and the Food and Drug Administration (FDA) collect data on antibiotic use in humans and in a more limited fashion in animals.[103]
The FDA first determined in 1977 that there is evidence of emergence of antibiotic-resistant bacterial strains in livestock. The long-established practice of permitting OTC sales of antibiotics (including penicillin and other drugs) to lay animal owners for administration to their own animals nonetheless continued in all states.
In 2000, the FDA announced their intention to revoke approval of fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone-resistant Campylobacter infections in humans. Legal challenges from the food animal and pharmaceutical industries delayed the final decision to do so until 2006.[104] Fluroquinolones have been banned from extra-label use in food animals in the USA since 2007. However, they remain widely used in companion and exotic animals.
Global action plans and awareness
The increasing interconnectedness of the world and the fact that new classes of antibiotics have not been developed and approved for more than 25 years highlight the extent to which antimicrobial resistance is a global health challenge.[105] A global action plan to tackle the growing problem of resistance to antibiotics and other antimicrobial medicines was endorsed at the Sixty-eighth World Health Assembly in May 2015.[106] One of the key objectives of the plan is to improve awareness and understanding of antimicrobial resistance through effective communication, education and training. This global action plan developed by the World Health Organization was created to combat the issue of antimicrobial resistance and was guided by the advice of countries and key stakeholders. The WHO's global action plan is composed of five key objectives that can be targeted through different means, and represents countries coming together to solve a major problem that can have future health consequences.[106]
- React based in Sweden has produced informative material on AMR for the general public.[107]
- Videos are being produced for the general public to generate interest and awareness.[108][109]
Antibiotic Awareness Week
The World Health Organization has promoted the first World Antibiotic Awareness Week running from 16–22 November 2015. The aim of the week is to increase global awareness of antibiotic resistance. It also wants to promote the correct usage of antibiotics across all fields in order to prevent further instances of antibiotic resistance.[110]
World Antibiotic Awareness Week has been held every November since 2015. For 2017, the Food and Agriculture Organization of the United Nations (FAO), the World Health Organization (WHO) and the World Organisation for Animal Health (OIE) are together calling for responsible use of antibiotics in humans and animals to reduce the emergence of antibiotic resistance.[111]
Mechanisms and organisms
Fundamentals
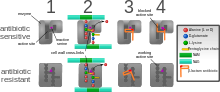
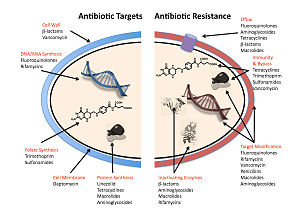
Diagram depicting antibiotic resistance through alteration of the antibiotic's target site, modeled after MRSA's resistance to penicillin. Beta-lactam antibiotics permanently inactivate PBP enzymes, which are essential for bacterial life, by permanently binding to their active sites. MRSA, however, expresses a PBP that does not allow the antibiotic into its active site.
The four main mechanisms by which microorganisms exhibit resistance to antimicrobials are:
- Drug inactivation or modification: for example, enzymatic deactivation of penicillin G in some penicillin-resistant bacteria through the production of β-lactamases. Most commonly, the protective enzymes produced by the bacterial cell will add an acetyl or phosphate group to a specific site on the antibiotic, which will reduce its ability to bind to the bacterial ribosomes and disrupt protein synthesis.[112]
- Alteration of target- or binding site: for example, alteration of PBP—the binding target site of penicillins—in MRSA and other penicillin-resistant bacteria. Another protective mechanism found among bacterial species is ribosomal protection proteins. These proteins protect the bacterial cell from antibiotics that target the cell’s ribosomes to inhibit protein synthesis. The mechanism involves the binding of the ribosomal protection proteins to the ribosomes of the bacterial cell, which in turn changes its conformational shape. This allows the ribosomes to continue synthesizing proteins essential to the cell while preventing antibiotics from binding to the ribosome to inhibit protein synthesis.[113]
- Alteration of metabolic pathway: for example, some sulfonamide-resistant bacteria do not require para-aminobenzoic acid (PABA), an important precursor for the synthesis of folic acid and nucleic acids in bacteria inhibited by sulfonamides, instead, like mammalian cells, they turn to using preformed folic acid.[114]
- Reduced drug accumulation: by decreasing drug permeability or increasing active efflux (pumping out) of the drugs across the cell surface[115] These pumps within the cellular membrane of certain bacterial species are used to pump antibiotics out of the cell before they are able to do any damage. They are often activated by a specific substrate associated with an antibiotic.[116] as in fluoroquinolone resistance.[117]
A number of mechanisms used by common antibiotics to deal with bacteria and ways by which bacteria become resistant to them.
Antibiotic resistance can be a result of horizontal gene transfer,[118] and also of unlinked point mutations in the pathogen genome at a rate of about 1 in 108 per chromosomal replication. Mutations are rare but the fact that bacteria reproduce at such a high rate allows for the effect to be significant. A mutation may produce a change in the binding site of the antibiotic, which may allow the site to continue proper functioning in the presence of the antibiotic or prevent the binding of the antibiotic to the site altogether.[119]
Antibiotic action against a pathogen can be seen as an environmental pressure. Those bacteria with a mutation that allows them to survive will reproduce, pass the trait to their offspring, which leads to the microevolution of a fully resistant colony. Chromosomal mutations providing antibiotic resistance benefit the bacteria but also confer a cost of fitness. For example, a ribosomal mutation may protect a bacterial cell by changing the binding site of an antibiotic but will also slow protein synthesis.[112] manifesting, in slower growth rate.[120]
In Gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase, protecting it from the action of quinolones. Finally, mutations at key sites in DNA gyrase or topoisomerase IV can decrease their binding affinity to quinolones, decreasing the drug's effectiveness.[121]
Bacteria

Klebsiella pneumoniae, the bacterium in which NDM-1 was first identified.
Bacteria can often develop antibiotic resistance. Mutations that confer increased survival are selected for in natural selection, which can happen quickly in bacteria because lifespans and production of new generations can be on a timescale of mere hours. A new (de novo) mutation in a parent cell can quickly become an inherited mutation of widespread prevalence. Moreover, some adaptive mutations can propagate not only through inheritance but also through horizontal gene transfer. Very often this is done via plasmids, however, through means of Transduction (genetics), Transformation (genetics) and chromosomal Conjugation (genetics), resistance genes residing on bacterial chromosomes can also be transferred. If the new DNA is maintained in the receiving bacterium, this transfer is followed by inheritance of the new resistance from parents to offspring.
Recent findings show no necessity of large populations of bacteria for the appearance of antibiotic resistance. Small populations of E. coli in an antibiotic gradient can become resistant. Any heterogeneous environment with respect to nutrient and antibiotic gradients may facilitate antibiotic resistance in small bacterial populations. Researchers hypothesize that the mechanism of resistance development is based on four SNP mutations in the genome of E. coli produced by the gradient of antibiotic.[122]
Antibiotic resistance can be introduced artificially into a microorganism through laboratory protocols, sometimes used as a selectable marker to examine the mechanisms of gene transfer or to identify individuals that absorbed a piece of DNA that included the resistance gene and another gene of interest.[123]
New Delhi metallo-beta-lactamase 1 (NDM-1)[124] is an enzyme that makes bacteria resistant to a broad range of beta-lactam antibiotics. The most common bacteria that make this enzyme are gram-negative such as Escherichia coli and Klebsiella pneumoniae, but the gene for NDM-1 can spread from one strain of bacteria to another by horizontal gene transfer.[125]
Viruses
Specific antiviral drugs are used to treat some viral infections. These drugs prevent viruses from reproducing by inhibiting essential stages of the virus's replication cycle in infected cells. Antivirals are used to treat HIV, hepatitis B, hepatitis C, influenza, herpes viruses including varicella zoster virus, cytomegalovirus and Epstein-Barr virus. With each virus, some strains have become resistant to the administered drugs.[126]
Resistance to HIV antivirals is problematic, and even multi-drug resistant strains have evolved.[127] Resistant strains of the HIV virus emerge rapidly if only one antiviral drug is used.[128] Using three or more drugs together has helped to control this problem, but new drugs are needed because of the continuing emergence of drug-resistant HIV strains.[129]
Fungi
Infections by fungi are a cause of high morbidity and mortality in immunocompromised persons, such as those with HIV/AIDS, tuberculosis or receiving chemotherapy.[130] The fungi candida, Cryptococcus neoformans and Aspergillus fumigatus cause most of these infections and antifungal resistance occurs in all of them.[131] Multidrug resistance in fungi is increasing because of the widespread use of antifungal drugs to treat infections in immunocompromised individuals.[132]
Of particular note, Fluconazole-resistant Candida species have been highlighted as a growing problem by the CDC.[82] More than 20 species of Candida can cause Candidiasis infection, the most common of which is Candida albicans. Candida yeasts normally inhabit the skin and mucous membranes without causing infection. However, overgrowth of Candida can lead to Candidiasis. Some Candida strains are becoming resistant to first-line and second-line antifungal agents such as azoles and echinocandins.[82]
Parasites
The protozoan parasites that cause the diseases malaria, trypanosomiasis, toxoplasmosis, cryptosporidiosis and leishmaniasis are important human pathogens.[133]
Malarial parasites that are resistant to the drugs that are currently available to infections are common and this has led to increased efforts to develop new drugs.[134] Resistance to recently developed drugs such as artemisinin has also been reported. The problem of drug resistance in malaria has driven efforts to develop vaccines.[135]
Trypanosomes are parasitic protozoa that cause African trypanosomiasis and Chagas disease (American trypanosomiasis).[136][137] There are no vaccines to prevent these infections so drugs such as pentamidine and suramin, benznidazole and nifurtimox are used to treat infections. These drugs are effective but infections caused by resistant parasites have been reported.[133]
Leishmaniasis is caused by protozoa and is an important public health problem worldwide, especially in sub-tropical and tropical countries. Drug resistance has "become a major concern".[138]
History
The discovery of penicillin in 1928 and other antibiotics in the 20th century proved to be a significant medical achievement, saving millions of lives and significantly reducing the burden of infectious diseases.[139] The 1950s to 1970s represented the golden age of antibiotic discovery, where countless new classes of antibiotics were discovered to treat previously incurable diseases such as tuberculosis and syphilis.[140] However, since that time the discovery of new classes of antibiotics has been almost nonexistent, and represents a situation that is especially problematic considering the resiliency of bacteria shown over time and the continued misuse and overuse of antibiotics in treatment.[141]
The phenomenon of antimicrobial resistance caused by overuse of antibiotics was predicted by Alexander Fleming who said "The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily under-dose himself and by exposing his microbes to nonlethal quantities of the drug make them resistant."[142][143] Without the creation of new and stronger antibiotics an era where common infections and minor injuries can kill, and where complex procedures such as surgery and chemotherapy become too risky, is a very real possibility.[144] Antimicrobial resistance threatens the world as we know it, and can lead to epidemics of enormous proportions if preventive actions are not taken. In this day and age current antimicrobial resistance leads to longer hospital stays, higher medical costs, and increased mortality.[141]
Society and culture
For the fiscal year 2016 budget, President Obama suggested to nearly double the amount of federal funding to "combat and prevent" antibiotic resistance to more than $1.2 billion.[145] Many international funding agencies like USAID, DFID, SIDA and Bill & Melinda Gates Foundation have pledged money for developing strategies to counter antimicrobial resistance.
Since the mid-1980s pharmaceutical companies have invested in medications for cancer or chronic disease that have greater potential to make money and have "de-emphasized or dropped development of antibiotics".[146] On January 20, 2016 at the World Economic Forum in Davos, Switzerland, more than "80 pharmaceutical and diagnostic companies" from around the world called for "transformational commercial models" at a global level to spur research and development on antibiotics and on the "enhanced use of diagnostic tests that can rapidly identify the infecting organism".[146]
Legal frameworks
Some global health scholars have argued that a global, legal framework is needed to prevent and control antimicrobial resistance.[147][148][19][149] For instance, binding global policies could be used to create antimicrobial use standards, regulate antibiotic marketing, and strengthen global surveillance systems.[19][147] Ensuring compliance of involved parties is a challenge.[19] Global antimicrobial resistance policies could take lessons from the environmental sector by adopting strategies that have made international environmental agreements successful in the past such as: sanctions for non-compliance, assistance for implementation, majority vote decision-making rules, an independent scientific panel, and specific commitments.[150]
U.S.
On March 27, 2015, the White House released a comprehensive plan to address the increasing need for agencies to combat the rise of antibiotic-resistant bacteria. The Task Force for Combating Antibiotic-Resistant Bacteria developed The National Action Plan for Combating Antibiotic-Resistant Bacteria with the intent of providing a roadmap to guide the US in the antibiotic resistance challenge and with hopes of saving many lives. This plan outlines steps taken by the Federal government over the next five years needed in order to prevent and contain outbreaks of antibiotic-resistant infections; maintain the efficacy of antibiotics already on the market; and to help to develop future diagnostics, antibiotics, and vaccines.[151]
The Action Plan was developed around five goals with focuses on strengthening health care, public health veterinary medicine, agriculture, food safety and research, and manufacturing. These goals, as listed by the White House, are as follows:
- Slow the Emergence of Resistant Bacteria and Prevent the Spread of Resistant Infections
- Strengthen National One-Health Surveillance Efforts to Combat Resistance
- Advance Development and use of Rapid and Innovative Diagnostic Tests for Identification and Characterization of Resistant Bacteria
- Accelerate Basic and Applied Research and Development for New Antibiotics, Other Therapeutics, and Vaccines
- Improve International Collaboration and Capacities for Antibiotic Resistance Prevention, Surveillance, Control and Antibiotic Research and Development
The following are goals set to meet by 2020:[151]
- Establishment of antimicrobial programs within acute care hospital settings
- Reduction of inappropriate antibiotic prescription and use by at least 50% in outpatient settings and 20% inpatient settings
- Establishment of State Antibiotic Resistance (AR) Prevention Programs in all 50 states
- Elimination of the use of medically important antibiotics for growth promotion in food-producing animals.
Policies
According to WHO policymakers can help tackle resistance by strengthening resistance tracking and laboratory capacity; regulating and promoting appropriate use of medicines.[22] Policymakers and industry can help tackle resistance by: fostering innovation and research and development of new tools; promoting cooperation and information sharing among all stakeholders.[22]
Further research
It is unclear if rapid viral testing affects antibiotic use in children.[152]
Vaccines
Microorganisms do not develop resistance to vaccines because a vaccine enhances the body's immune system, whereas an antibiotic operates separately from the body's normal defenses. Furthermore, if the use of vaccines increases, there is evidence that antibiotic resistant strains of pathogens will decrease; the need for antibiotics will naturally decrease as vaccines prevent infection before it occurs.[153] However, new strains that escape immunity induced by vaccines may evolve; for example, an updated influenza vaccine is needed each year.
While theoretically promising, antistaphylococcal vaccines have shown limited efficacy, because of immunological variation between Staphylococcus species, and the limited duration of effectiveness of the antibodies produced. Development and testing of more effective vaccines is underway.[154]
Alternating therapy
Alternating therapy is a proposed method in which two or three antibiotics are taken in a rotation versus taking just one antibiotic such that bacteria resistant to one antibiotic are killed when the next antibiotic is taken. Studies have found that this method reduces the rate at which antibiotic resistant bacteria emerge in vitro relative to a single drug for the entire duration.[155]
Studies have found that bacteria that evolve antibiotic resistance towards one group of antibiotic may become more sensitive to others.[156] This phenomenon can be utilized to select against resistant bacteria using an approach termed collateral sensitivity cycling,[157] which has recently been found to be relevant in developing treatment strategies for chronic infections caused by Pseudomonas aeruginosa.[158]
Development of new drugs
Since the discovery of antibiotics, research and development (R&D) efforts have provided new drugs in time to treat bacteria that became resistant to older antibiotics, but in the 2000s there has been concern that development has slowed enough that seriously ill people may run out of treatment options.[159][160] Another concern is that doctors may become reluctant to perform routine surgeries because of the increased risk of harmful infection.[161] Backup treatments can have serious side-effects; for example, treatment of multi-drug-resistant tuberculosis can cause deafness or psychological disability.[162] The potential crisis at hand is the result of a marked decrease in industry R&D.[163] Poor financial investment in antibiotic research has exacerbated the situation.[164][163] The pharmaceutical industry has little incentive to invest in antibiotics because of the high risk and because the potential financial returns are less likely to cover the cost of development than for other pharmaceuticals.[165] In 2011, Pfizer, one of the last major pharmaceutical companies developing new antibiotics, shut down its primary research effort, citing poor shareholder returns relative to drugs for chronic illnesses.[166] However, small and medium-sized pharmaceutical companies are still active in antibiotic drug research.
In the United States, drug companies and the administration of President Barack Obama have been proposing changing the standards by which the FDA approves antibiotics targeted at resistant organisms.[161][167] On 12 December 2013, the Antibiotic Development to Advance Patient Treatment (ADAPT) Act of 2013 was introduced in the U.S. Congress. The ADAPT Act aims to fast-track the drug development in order to combat the growing public health threat of 'superbugs'. Under this Act, the FDA can approve antibiotics and antifungals needed for life-threatening infections based on data from smaller clinical trials. The Centers for Disease Control and Prevention (CDC) will reinforce the monitoring of the use of antibiotics that treat serious and life-threatening infections and the emerging resistance, and make the data publicly available. The FDA antibiotics labeling process, 'Susceptibility Test Interpretive Criteria for Microbial Organisms' or 'breakpoints' is also streamlined to allow the most up-to-date and cutting-edge data available to healthcare professionals under the new Act.[168][169]
On 18 September 2014 Obama signed an executive order[170] to implement the recommendations proposed in a report[171] by the President's Council of Advisors on Science and Technology (PCAST) which outlines strategies to stream-line clinical trials and speed up the R&D of new antibiotics. Among the proposals:
- Create a 'robust, standing national clinical trials network for antibiotic testing' which will promptly enroll patients once identified to be suffering from dangerous bacterial infections. The network will allow testing multiple new agents from different companies simultaneously for their safety and efficacy.
- Establish a 'Special Medical Use (SMU)' pathway for FDA to approve new antimicrobial agents for use in limited patient populations, shorten the approval timeline for new drug so patients with severe infections could benefit as quickly as possible.
- Provide economic incentives, especially for development of new classes of antibiotics, to offset the steep R&D costs which drive away the industry to develop antibiotics.
Rapid diagnostics
Antimicrobial susceptibility testing (AST) can help practitioners avoid prescribing unnecessary antibiotics in the style of precision medicine,[172] and help them prescribe effective antibiotics, but with the traditional approach it could take 12 to 48 hours.[173] Rapid testing, possible from molecular diagnostics innovations, is defined as "being feasible within an 8-h working shift".[173] Progress has been slow due to a range of reasons including cost and regulation.[174]
Phage therapy
Phage therapy is the therapeutic use of bacteriophages to treat pathogenic bacterial infections.[175] Phage therapy has many potential applications in human medicine as well as dentistry, veterinary science, and agriculture.[176]
Phage therapy relies on the use of naturally-occurring bacteriophages to infect and lyse bacteria at the site of infection in a host. Due to current advances in genetics and biotechnology these bacteriophages can possibly be manufactured to treat specific infections.[177] Phages can be bioengineered to target multidrug-resistant bacterial infections, and their use involves the added benefit of preventing the elimination of beneficial bacteria in the human body.[177] Phages destroy bacterial cell walls and membrane through the use of lytic proteins which kill bacteria by making many holes from the inside out.[178] Bacteriophages can even possess the ability to digest the biofilm that many bacteria develop that protect them from antibiotics in order to effectively infect and kill bacteria. Bioengineering can play a role in creating successful bacteriophages.[178]
Understanding the mutual interactions and evolutions of bacterial and phage populations in the environment of a human or animal body is essential for rational phage therapy.[179]
Bacteriophagics are used against antibiotic resistant bacteria in Georgia (George Eliava Institute) and in one institute in Wrocław, Poland.[180][181] Bacteriophage cocktails are common drugs sold over the counter in pharmacies in eastern countries.[182][183]
See also
- Alliance for the Prudent Use of Antibiotics
- Broad-spectrum antibiotic
- Colonisation resistance
- Drug of last resort
- Genetic engineering
- (KPC) antibacterial resistance gene
- Multidrug tolerance
- Multidrug-resistant Gram-negative bacteria
Resistance-nodulation-cell division superfamily (RND)- Resistome
References
^ Kirby-Bauer Disk Diffusion Susceptibility Test Protocol Archived 2011-06-26 at the Wayback Machine., Jan Hudzicki, ASM
^ "Review on Antimicrobial Resistance". amr-review.org. Archived from the original on 25 September 2015. Retrieved 20 May 2016..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output q{quotes:"""""""'""'"}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ abc "Antimicrobial resistance Fact sheet N°194". who.int. April 2014. Archived from the original on 10 March 2015. Retrieved 7 March 2015.
^ "About Antimicrobial Resistance - Antibiotic/Antimicrobial Resistance - CDC". www.cdc.gov. 19 September 2017. Archived from the original on 1 October 2017. Retrieved 8 September 2017.
^ "Antibiotic Resistance Questions & Answers". Get Smart: Know When Antibiotics Work. Centers for Disease Control and Prevention, USA. 30 June 2009. Archived from the original on 29 March 2013. Retrieved 20 March 2013.
^ "General Background: About Antibiotic Resistance". www.tufts.edu. Archived from the original on 23 October 2015. Retrieved 30 October 2015.
^ ab Goossens H, Ferech M, Vander Stichele R, Elseviers M (2005). "Outpatient antibiotic use in Europe and association with resistance: a cross-national database study". Lancet. 365 (9459): 579–87. doi:10.1016/S0140-6736(05)17907-0. PMID 15708101.
(subscription required)
^ abc "About Antimicrobial Resistance". www.cdc.gov. 10 September 2018. Archived from the original on 1 October 2017. Retrieved 30 October 2015.
^ ab Swedish work on containment of antibiotic resistance – Tools, methods and experiences (PDF). Stockholm: Public Health Agency of Sweden. 2014. pp. 16–17, 121–128. ISBN 978-91-7603-011-0. Archived (PDF) from the original on 23 July 2015. Retrieved 23 July 2015.
^ abcdef "Duration of antibiotic therapy and resistance". NPS Medicinewise. National Prescribing Service Limited trading, Australia. 13 June 2013. Archived from the original on 23 July 2015. Retrieved 22 July 2015.
^ ab "CDC Features – Mission Critical: Preventing Antibiotic Resistance". www.cdc.gov. 4 April 2018. Archived from the original on 8 November 2017. Retrieved 22 July 2015.
^ Changing Markets. "IMPACTS OF PHARMACEUTICAL POLLUTION ON COMMUNITIES AND ENVIRONMENT IN INDIA" (PDF). Nordea. Nordea. Archived (PDF) from the original on 20 May 2017. Retrieved 1 May 2018.
^ Gullberg E, Cao S, Berg OG, Ilbäck C, Sandegren L, Hughes D, Andersson DI (July 2011). "Selection of resistant bacteria at very low antibiotic concentrations". PLoS Pathogens. 7 (7): e1002158. doi:10.1371/journal.ppat.1002158. PMC 3141051. PMID 21811410.
^ Cassir N, Rolain JM, Brouqui P (2014). "A new strategy to fight antimicrobial resistance: the revival of old antibiotics". Frontiers in Microbiology. 5: 551. doi:10.3389/fmicb.2014.00551. PMC 4202707. PMID 25368610.
^ Sample I (26 March 2018). "Calls to rein in antibiotic use after study shows 65% increase worldwide". The Guardian. Archived from the original on 8 April 2018. Retrieved 28 March 2018.
^ WHO (April 2014). "Antimicrobial resistance: global report on surveillance 2014". WHO. WHO. Archived from the original on 15 May 2015. Retrieved 9 May 2015.
^ ab O'neill J (May 2016). "TACKLING DRUG-RESISTANT INFECTIONS GLOBALLY: FINAL REPORT AND RECOMMENDATIONS" (PDF). amr-review.org/. Archived (PDF) from the original on 14 November 2017. Retrieved 10 November 2017.
^ "Antibiotic / Antimicrobial Resistance - CDC". www.cdc.gov. 18 August 2017. Archived from the original on 7 October 2016. Retrieved 6 October 2016.
^ abcd Hoffman SJ, Outterson K, Røttingen JA, Cars O, Clift C, Rizvi Z, Rotberg F, Tomson G, Zorzet A (February 2015). "An international legal framework to address antimicrobial resistance". Bulletin of the World Health Organization. 93 (2): 66. doi:10.2471/BLT.15.152710. PMC 4339972. PMID 25883395.
^ "What is Drug Resistance?". www.niaid.nih.gov. Archived from the original on 27 July 2015. Retrieved 26 July 2015.
^ "CDC: Get Smart: Know When Antibiotics Work". Cdc.gov. 29 May 2018. Archived from the original on 29 April 2015. Retrieved 12 June 2013.
^ abcde "WHO's first global report on antibiotic resistance reveals serious, worldwide threat to public health" Archived 2 May 2014 at the Wayback Machine. Retrieved 2014-05-02
^ "Antibiotic-resistant bacteria responsible for over 33,000 deaths in Europe in 2015, study finds". Pharmaceutical Journal. 7 November 2018. Retrieved 16 December 2018.
^ D'Costa VM, King CE, Kalan L, Morar M, Sung WW, Schwarz C, Froese D, Zazula G, Calmels F, Debruyne R, Golding GB, Poinar HN, Wright GD (August 2011). "Antibiotic resistance is ancient". Nature. 477 (7365): 457–61. Bibcode:2011Natur.477..457D. doi:10.1038/nature10388. PMID 21881561.
^ Caldwell & Lindberg 2011.
^ Hawkey & Jones 2009, pp. i3-i10.
^ Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H, Greko C, So AD, Bigdeli M, Tomson G, Woodhouse W, Ombaka E, Peralta AQ, Qamar FN, Mir F, Kariuki S, Bhutta ZA, Coates A, Bergstrom R, Wright GD, Brown ED, Cars O (December 2013). "Antibiotic resistance-the need for global solutions". The Lancet. Infectious Diseases. 13 (12): 1057–98. doi:10.1016/S1473-3099(13)70318-9. hdl:10161/8996. PMID 24252483. As PDF Archived 24 September 2015 at the Wayback Machine..
^ Ferber D (January 2002). "Antibiotic resistance. Livestock feed ban preserves drugs' power". Science. 295 (5552): 27–8. doi:10.1126/science.295.5552.27a. PMID 11778017.
(subscription required)
^ Mathew AG, Cissell R, Liamthong S (2007). "Antibiotic resistance in bacteria associated with food animals: a United States perspective of livestock production". Foodborne Pathogens and Disease. 4 (2): 115–33. doi:10.1089/fpd.2006.0066. PMID 17600481.
^ "Pharmaceuticals Sold In Sweden Cause Serious Environmental Harm In India, Research Shows". ScienceDaily. ScienceDaily, LLC. 7 February 2009. Archived from the original on 4 February 2015. Retrieved 29 January 2015.We estimated that the[water] treatment plant released 45 kilograms of the antibiotic ciprofloxacin in one day, which is equivalent to five times the daily consumption of Sweden,”
^ Joakim Larsson DG, Fick J (April 2009). "Transparency throughout the production chain--a way to reduce pollution from the manufacturing of pharmaceuticals?". Regulatory Toxicology and Pharmacology. 53 (3): 161–3. doi:10.1016/j.yrtph.2009.01.008. PMID 19545507.
(subscription required)
^ CDC (29 May 2018). "Antibiotic Resistance Questions and Answers" [Are antibacterial-containing products (soaps, household cleaners, etc.) better for preventing the spread of infection? Does their use add to the problem of resistance?]. Atlanta, Georgia, USA.: Centers for Disease Control and Prevention. Archived from the original on 29 April 2015. Retrieved 25 February 2015.
^ Aiello AE, Larson EL, Levy SB (September 2007). "Consumer antibacterial soaps: effective or just risky?". Clinical Infectious Diseases. 45 Suppl 2 (Supplement 2): S137–47. doi:10.1086/519255. PMID 17683018.
^ Shepherd MJ, Moore G, Wand ME, Sutton JM, Bock LJ (November 2018). "Pseudomonas aeruginosa adapts to octenidine in the laboratory and a simulated clinical setting, leading to increased tolerance to chlorhexidine and other biocides". The Journal of Hospital Infection. 100 (3): e23–e29. doi:10.1016/j.jhin.2018.03.037. PMID 29614247.
^ Wand ME, Bock LJ, Bonney LC, Sutton JM (January 2017). "Mechanisms of Increased Resistance to Chlorhexidine and Cross-Resistance to Colistin following Exposure of Klebsiella pneumoniae Clinical Isolates to Chlorhexidine". Antimicrobial Agents and Chemotherapy. 61 (1). doi:10.1128/AAC.01162-16. PMC 5192135. PMID 27799211.
^ Pechère JC (September 2001). "Patients' interviews and misuse of antibiotics". Clinical Infectious Diseases. 33 Suppl 3: S170–3. CiteSeerX 10.1.1.560.8090. doi:10.1086/321844. PMID 11524715.Noncompliance may have an impact on antibiotic resistance ... Type A consists in shorter than prescribed courses. By reducing the antibiotic pressure, provided that the daily doses are otherwise respected, one may see a theoretical advantage ... Type B noncompliance reduces the number of daily doses ... indicate that such underdosing may promote the selection of resistance
^ Arnold SR, Straus SE (October 2005). Arnold SR, ed. "Interventions to improve antibiotic prescribing practices in ambulatory care". The Cochrane Database of Systematic Reviews (4): CD003539. doi:10.1002/14651858.CD003539.pub2. PMID 16235325.
^ abcdefg Araya P (May 2016). "The Impact of Water and Sanitation on Diarrhoeal Disease Burden and Over-Consumption of Anitbiotics" (PDF). Archived (PDF) from the original on 1 October 2017. Retrieved 12 November 2017.
^ Ventola, C. Lee. "The antibiotic resistance crisis: part 1: causes and threats." Pharmacy and Therapeutics 40.4 (2015): 277.
^ McNulty CA, Boyle P, Nichols T, Clappison P, Davey P (August 2007). "The public's attitudes to and compliance with antibiotics". The Journal of Antimicrobial Chemotherapy. 60 Suppl 1: i63–8. doi:10.1093/jac/dkm161. PMID 17656386.
(subscription required)
^ Eccles R, Weber O, eds. (2009). Common cold (Online ed.). Basel: Birkhäuser. p. 234. ISBN 978-3-7643-9894-1.
^ Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD (May 2010). "Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis". BMJ. 340: c2096. doi:10.1136/bmj.c2096. PMID 20483949.
(subscription required)
^ Antimicrobial Resistance: Tackling a Crises for the Health and Welfare of Nations: 2014 (PDF). London. 11 December 2014. Archived (PDF) from the original on 3 May 2018. Retrieved 24 April 2018.
^ Li JZ, Winston LG, Moore DH, Bent S (September 2007). "Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis". The American Journal of Medicine. 120 (9): 783–90. doi:10.1016/j.amjmed.2007.04.023. PMID 17765048.
(subscription required)
^ Runyon BA, McHutchison JG, Antillon MR, Akriviadis EA, Montano AA (June 1991). "Short-course versus long-course antibiotic treatment of spontaneous bacterial peritonitis. A randomized controlled study of 100 patients". Gastroenterology. 100 (6): 1737–42. PMID 2019378.
(subscription required)
^ Singh N, Rogers P, Atwood CW, Wagener MM, Yu VL (August 2000). "Short-course empiric antibiotic therapy for patients with pulmonary infiltrates in the intensive care unit. A proposed solution for indiscriminate antibiotic prescription". American Journal of Respiratory and Critical Care Medicine. 162 (2 Pt 1): 505–11. doi:10.1164/ajrccm.162.2.9909095. PMID 10934078.
(subscription required)
^ Gleisner AL, Argenta R, Pimentel M, Simon TK, Jungblut CF, Petteffi L, de Souza RM, Sauerssig M, Kruel CD, Machado AR (May 2004). "Infective complications according to duration of antibiotic treatment in acute abdomen". International Journal of Infectious Diseases. 8 (3): 155–62. doi:10.1016/j.ijid.2003.06.003. PMID 15109590.
(subscription required)
^ Pichichero ME, Cohen R (July 1997). "Shortened course of antibiotic therapy for acute otitis media, sinusitis and tonsillopharyngitis". The Pediatric Infectious Disease Journal. 16 (7): 680–95. doi:10.1097/00006454-199707000-00011. PMID 9239773.
(subscription required)
^ Dellinger EP, Wertz MJ, Lennard ES, Oreskovich MR (January 1986). "Efficacy of short-course antibiotic prophylaxis after penetrating intestinal injury. A prospective randomized trial". Archives of Surgery. 121 (1): 23–30. doi:10.1001/archsurg.1986.01400010029002. PMID 3942496.
(subscription required)
^ Perez-Gorricho B, Ripoll M (March 2003). "Does short-course antibiotic therapy better meet patient expectations?". International Journal of Antimicrobial Agents. 21 (3): 222–8. doi:10.1016/S0924-8579(02)00360-6. PMID 12636982.
(subscription required)
^ Keren R, Chan E (May 2002). "A meta-analysis of randomized, controlled trials comparing short- and long-course antibiotic therapy for urinary tract infections in children". Pediatrics. 109 (5): E70–0. doi:10.1542/peds.109.5.e70. PMID 11986476.
(subscription required)
^ McCormack J, Allan GM (February 2012). "A prescription for improving antibiotic prescribing in primary care". BMJ. 344: d7955. doi:10.1136/bmj.d7955. PMID 22302779.
(subscription required)
^ Marc Bonten, MD; Eijkman-Winkler Institute for Medical Microbiology, Utrecht, the Netherland | Infectious Diseases, and Inflammation Archived 17 May 2013 at the Wayback Machine.
^ Tacconelli E, De Angelis G, Cataldo MA, Pozzi E, Cauda R (January 2008). "Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis". The Journal of Antimicrobial Chemotherapy. 61 (1): 26–38. doi:10.1093/jac/dkm416. PMID 17986491.
(subscription required)
^ Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, Farr BM (May 2003). "SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus" (PDF). Infection Control and Hospital Epidemiology. 24 (5): 362–86. CiteSeerX 10.1.1.575.8929. doi:10.1086/502213. PMID 12785411. Archived (PDF) from the original on 18 April 2016. Retrieved 24 October 2017.
^ Vonberg R. "Clostridium difficile: a challenge for hospitals". European Center for Disease Prevention and Control. Institute for Medical Microbiology and Hospital Epidemiology: IHE. Archived from the original on 11 June 2009. Retrieved 27 July 2009.
^ Kuijper EJ, van Dissel JT, Wilcox MH (August 2007). "Clostridium difficile: changing epidemiology and new treatment options". Current Opinion in Infectious Diseases. 20 (4): 376–83. doi:10.1097/QCO.0b013e32818be71d. PMID 17609596.
^ Thomas JK, Forrest A, Bhavnani SM, Hyatt JM, Cheng A, Ballow CH, Schentag JJ (March 1998). "Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy". Antimicrobial Agents and Chemotherapy. 42 (3): 521–7. PMC 105492. PMID 9517926.
(subscription required)
^ Girou E, Legrand P, Soing-Altrach S, Lemire A, Poulain C, Allaire A, Tkoub-Scheirlinck L, Chai SH, Dupeyron C, Loche CM (October 2006). "Association between hand hygiene compliance and methicillin-resistant Staphylococcus aureus prevalence in a French rehabilitation hospital". Infection Control and Hospital Epidemiology. 27 (10): 1128–30. doi:10.1086/507967. PMID 17006822.
(subscription required)
^ "Fake drugs: the global industry putting your life at risk". Mosaic. 30 October 2018. Retrieved 13 December 2018.
^ "Antibiotic resistance". World Health Organization. Archived from the original on 20 April 2016. Retrieved 21 April 2016.
^ "1.6.7". Access online: OIE - World Organisation for Animal Health. www.oie.int. Archived from the original on 3 December 2013. Retrieved 14 November 2015.
^ "1.6.8". Access online: OIE - World Organisation for Animal Health. www.oie.int. Archived from the original on 3 December 2013. Retrieved 14 November 2015.
^ "1.6.9". Access online: OIE - World Organisation for Animal Health. www.oie.int. Archived from the original on 3 December 2013. Retrieved 14 November 2015.
^ abc Wright GD (October 2010). "Antibiotic resistance in the environment: a link to the clinic?". Current Opinion in Microbiology. 13 (5): 589–94. doi:10.1016/j.mib.2010.08.005. PMID 20850375.
(subscription required)
^ D'Costa VM, King CE, Kalan L, Morar M, Sung WW, Schwarz C, Froese D, Zazula G, Calmels F, Debruyne R, Golding GB, Poinar HN, Wright GD (August 2011). "Antibiotic resistance is ancient". Nature. 477 (7365): 457–61. Bibcode:2011Natur.477..457D. doi:10.1038/nature10388. PMID 21881561.
^ Pawlowski AC, Wang W, Koteva K, Barton HA, McArthur AG, Wright GD (December 2016). "A diverse intrinsic antibiotic resistome from a cave bacterium". Nature Communications. 7: 13803. Bibcode:2016NatCo...713803P. doi:10.1038/ncomms13803. PMC 5155152. PMID 27929110.
^ "Mutations are random". University of California. Archived from the original on 8 February 2012. Retrieved 14 August 2011.
^ Richard William Nelson. Darwin, Then and Now: The Most Amazing Story in the History of Science, i Universe, 2009, p. 294
^ Kiser JS, Gale GO, Kemp GA (1970). "3.2 Resistance to Antimicrobial Agents: Evolution of Drug Resistance". Advances in Applied Microbiology. 11. Academic Press. p. 80. ISBN 978-0-08-056425-8.
^ Pollock MR (October 1967). "Origin and function of penicillinase: a problem in biochemical evolution". British Medical Journal. 4 (5571): 71–7. doi:10.1136/bmj.4.5571.71. PMC 1748446. PMID 4963324.
(subscription required)
^ ab Information, Reed Business (8 June 1972). "Some bacteria choose to live in a pool of penicillin". New Scientist. 54 (799): 546.
^ ab Siddal R (11 February 1989). "Ancient bacteria resitent to some antibiotics". New Scientist. 121 (1651): 34. Bibcode:1989NewSc.121...34H.
^ Pollock, p. 77
^ Seiler C, Berendonk TU (December 14, 2012). "Heavy metal driven co-selection of antibiotic resistance in soil and water bodies impacted by agriculture and aquaculture". Frontiers in Microbiology. 3: 399. doi:10.3389/fmicb.2012.00399. PMC 3522115. PMID 23248620.
^ Levy SB (January 2002). "The 2000 Garrod lecture. Factors impacting on the problem of antibiotic resistance". The Journal of Antimicrobial Chemotherapy. 49 (1): 25–30. doi:10.1093/jac/49.1.25. PMID 11751763.
^ Marti E, Variatza E, Balcazar JL (January 2014). "The role of aquatic ecosystems as reservoirs of antibiotic resistance". Trends in Microbiology. 22 (1): 36–41. doi:10.1016/j.tim.2013.11.001. PMID 24289955. Archived from the original on 10 May 2017. Retrieved 9 December 2016.
^ ab Martinez, J. L., & Olivares, J. (2012).
Environmental Pollution By Antibiotic Resistance Genes. In P. L. Keen, & M. H. Montforts, Antimicrobial Resistance in the Environment (pp. 151- 171). Hoboken, N.J.: John Wiley & Sons.
^ Yezli S, Li H (November 2012). "Antibiotic resistance amongst healthcare-associated pathogens in China". International Journal of Antimicrobial Agents. 40 (5): 389–97. doi:10.1016/j.ijantimicag.2012.07.009. PMID 22999767.
^ Walsh TR, Weeks J, Livermore DM, Toleman MA (May 2011). "Dissemination of NDM-1 positive bacteria in the New Delhi environment and its implications for human health: an environmental point prevalence study". The Lancet. Infectious Diseases. 11 (5): 355–62. doi:10.1016/S1473-3099(11)70059-7. PMID 21478057.
^ Rose JM, Gast RJ, Bogomolni A, Ellis JC, Lentell BJ, Touhey K, Moore M (March 2009). "Occurrence and patterns of antibiotic resistance in vertebrates off the Northeastern United States coast". FEMS Microbiology Ecology. 67 (3): 421–31. doi:10.1111/j.1574-6941.2009.00648.x. PMC 5444207. PMID 19187217.
^ abc "Biggest Threats - Antibiotic/Antimicrobial Resistance - CDC". www.cdc.gov. 10 September 2018. Archived from the original on 12 September 2017. Retrieved 5 May 2016.
^ "HealthMap Resistance". HealthMap.org Boston Children’s Hospital. Archived from the original on 15 November 2017. Retrieved 15 November 2017.
^ Scales D. "Mapping Antibiotic Resistance: Know The Germs In Your Neighborhood". WBUR. National Public Radio. Archived from the original on 8 December 2015. Retrieved 8 December 2015.
^ "ResistanceMap". Center for Disease Dynamics, Economics & Policy. Archived from the original on 14 November 2017. Retrieved 14 November 2017.
^ Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Döbele S, Tacconelli E (September 2017). "Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis". The Lancet. Infectious Diseases. 17 (9): 990–1001. doi:10.1016/S1473-3099(17)30325-0. PMID 28629876.
^ Andersson DI, Hughes D (September 2011). "Persistence of antibiotic resistance in bacterial populations". FEMS Microbiology Reviews. 35 (5): 901–11. doi:10.1111/j.1574-6976.2011.00289.x. PMID 21707669.
^ Gilberg K, Laouri M, Wade S, Isonaka S (2003). "Analysis of medication use patterns:apparent overuse of antibiotics and underuse of prescription drugs for asthma, depression, and CHF". Journal of Managed Care Pharmacy. 9 (3): 232–7. doi:10.18553/jmcp.2003.9.3.232. PMID 14613466.
^ Doron S, Davidson LE (November 2011). "Antimicrobial stewardship". Mayo Clinic Proceedings. 86 (11): 1113–23. doi:10.4065/mcp.2011.0358. PMC 3203003. PMID 22033257.
^ Davey P, Marwick CA, Scott CL, Charani E, McNeil K, Brown E, Gould IM, Ramsay CR, Michie S (February 2017). "Interventions to improve antibiotic prescribing practices for hospital inpatients". The Cochrane Database of Systematic Reviews. 2: CD003543. doi:10.1002/14651858.cd003543.pub4. PMID 28178770.
^ O'Sullivan JW, Harvey RT, Glasziou PP, McCullough A (November 2016). "Written information for patients (or parents of child patients) to reduce the use of antibiotics for acute upper respiratory tract infections in primary care". The Cochrane Database of Systematic Reviews. 11: CD011360. doi:10.1002/14651858.CD011360.pub2. PMID 27886368.
^ "The Five Rights of Medication Administration". www.ihi.org. Archived from the original on 24 October 2015. Retrieved 30 October 2015.
^ Leekha S, Terrell CL, Edson RS (February 2011). "General principles of antimicrobial therapy". Mayo Clinic Proceedings. 86 (2): 156–67. doi:10.4065/mcp.2010.0639. PMC 3031442. PMID 21282489.
^ Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File TM, Finkelstein JA, Gerber JS, Hyun DY, Linder JA, Lynfield R, Margolis DJ, May LS, Merenstein D, Metlay JP, Newland JG, Piccirillo JF, Roberts RM, Sanchez GV, Suda KJ, Thomas A, Woo TM, Zetts RM, Hicks LA (May 2016). "Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011". JAMA. 315 (17): 1864–73. doi:10.1001/jama.2016.4151. PMID 27139059.
^ "Indicator: Antibiotic prescribing". QualityWatch. Nuffield Trust & Health Foundation. Archived from the original on 14 January 2015. Retrieved 16 July 2015.
^ abc IACG (2018) Reduce unintentional exposure and the need for antimicrobials, and optimize their use IACG Discussion Paper, Interagency Coordination Group on Antimicrobial Resistance, public consultation process at WHO, Geneva, Switzerland
^ Swoboda SM, Earsing K, Strauss K, Lane S, Lipsett PA (February 2004). "Electronic monitoring and voice prompts improve hand hygiene and decrease nosocomial infections in an intermediate care unit". Critical Care Medicine. 32 (2): 358–63. doi:10.1097/01.CCM.0000108866.48795.0F. PMID 14758148.
(subscription required)
^ WHO, UNICEF (2015). Water, sanitation and hygiene in health care facilities - Status in low and middle income countries and way forward Archived 12 September 2018 at the Wayback Machine.. World Health Organization (WHO), Geneva, Switzerland,
ISBN 978 92 4 150847 6
^ Casewell M, Friis C, Marco E, McMullin P, Phillips I (August 2003). "The European ban on growth-promoting antibiotics and emerging consequences for human and animal health". The Journal of Antimicrobial Chemotherapy. 52 (2): 159–61. doi:10.1093/jac/dkg313. PMID 12837737.
^ Castanon JI (November 2007). "History of the use of antibiotic as growth promoters in European poultry feeds". Poultry Science. 86 (11): 2466–71. doi:10.3382/ps.2007-00249. PMID 17954599.
(subscription required)
^ Bengtsson B, Wierup M (2006). "Antimicrobial resistance in Scandinavia after ban of antimicrobial growth promoters". Animal Biotechnology. 17 (2): 147–56. doi:10.1080/10495390600956920. PMID 17127526.
(subscription required)
^ Angulo FJ, Baker NL, Olsen SJ, Anderson A, Barrett TJ (April 2004). "Antimicrobial use in agriculture: controlling the transfer of antimicrobial resistance to humans". Seminars in Pediatric Infectious Diseases. 15 (2): 78–85. doi:10.1053/j.spid.2004.01.010. PMID 15185190. Archived from the original on 2 June 2018. Retrieved 4 March 2017.
^ "GAO-11-801, Antibiotic Resistance: Agencies Have Made Limited Progress Addressing Antibiotic Use in Animals". gao.gov. Archived from the original on 5 November 2013. Retrieved 25 January 2014.
^ Nelson JM, Chiller TM, Powers JH, Angulo FJ (April 2007). "Fluoroquinolone-resistant Campylobacter species and the withdrawal of fluoroquinolones from use in poultry: a public health success story". Clinical Infectious Diseases. 44 (7): 977–80. doi:10.1086/512369. PMID 17342653.
^ "RAND Europe Focus on Antimicrobial Resistance (AMR)". www.rand.org. Archived from the original on 21 April 2018. Retrieved 23 April 2018.
^ ab WHO. "GLOBAL ACTION PLAN ON ANTIMICROBIAL RESISTANCE" (PDF). Archived (PDF) from the original on 31 October 2017. Retrieved 14 November 2017.
^ "React". Archived from the original on 16 November 2017. Retrieved 16 November 2017.
^ "Antibiotic Resistance: the silent tsunami (youtube video)". ReActTube. 6 March 2017. Retrieved 17 November 2017.
^ "The Antibiotic Apocalypse Explained". Kurzgesagt – In a Nutshell. 16 March 2016. Retrieved 17 November 2017.
^ "World Antibiotic Awareness Week". World Health Organization. Archived from the original on 20 November 2015. Retrieved 20 November 2015.
^ "World Antibiotic Awareness Week". WHO. Archived from the original on 13 November 2017. Retrieved 14 November 2017.
^ ab [Criswell, Daniel. "The "Evolution" of Antibiotic Resistance." Institute for Creation Research. N.p., 2004. Web. 28 Oct. 2014.]
^ Connell SR, Tracz DM, Nierhaus KH, Taylor DE (December 2003). "Ribosomal protection proteins and their mechanism of tetracycline resistance". Antimicrobial Agents and Chemotherapy. 47 (12): 3675–81. doi:10.1128/AAC.47.12.3675-3681.2003. PMC 296194. PMID 14638464. Archived from the original on 1 June 2018. Retrieved 14 June 2018.
^ Henry, Richard J. (December 1943). "THE MODE OF ACTION OF SULFONAMIDES *". Bacteriological Reviews. 7 (4): 175–262. ISSN 0005-3678. PMC 440870. PMID 16350088.
^ Li XZ, Nikaido H (August 2009). "Efflux-mediated drug resistance in bacteria: an update". Drugs. 69 (12): 1555–623. doi:10.2165/11317030-000000000-00000. PMC 2847397. PMID 19678712.
^ [RI Aminov, RI Mackie. Evolution and ecology of antibiotic resistance genes. Microbiology Letters. 8 May 2007. doi:10.1111/j.1574-6968.2007.00757.x]
^ Morita Y, Kodama K, Shiota S, Mine T, Kataoka A, Mizushima T, Tsuchiya T (July 1998). "NorM, a putative multidrug efflux protein, of Vibrio parahaemolyticus and its homolog in Escherichia coli". Antimicrobial Agents and Chemotherapy. 42 (7): 1778–82. PMC 105682. PMID 9661020.
^ Ochiai K, Yamanaka T, Kimura K, Sawada O, O (1959). "Inheritance of drug resistance (and its transfer) between Shigella strains and Between Shigella and E.coli strains". Hihon Iji Shimpor (in Japanese). 34: 1861.
^ Cirz RT, Chin JK, Andes DR, de Crécy-Lagard V, Craig WA, Romesberg FE (June 2005). "Inhibition of mutation and combating the evolution of antibiotic resistance". PLoS Biology. 3 (6): e176. doi:10.1371/journal.pbio.0030176. PMC 1088971. PMID 15869329.
^ Levin BR, Perrot V, Walker N (March 2000). "Compensatory mutations, antibiotic resistance and the population genetics of adaptive evolution in bacteria". Genetics. 154 (3): 985–97. PMC 1460977. PMID 10757748.
^ Robicsek A, Jacoby GA, Hooper DC (October 2006). "The worldwide emergence of plasmid-mediated quinolone resistance". The Lancet. Infectious Diseases. 6 (10): 629–40. doi:10.1016/S1473-3099(06)70599-0. PMID 17008172.
^ Johansen TB, Scheffer L, Jensen VK, Bohlin J, Feruglio SL (June 2018). "Whole-genome sequencing and antimicrobial resistance in Brucella melitensis from a Norwegian perspective". Scientific Reports. 8 (1): 8538. doi:10.1038/s41598-018-26906-3. PMC 5986768. PMID 29867163.
^ Chan CX, Beiko RG, Ragan MA (August 2011). "Lateral transfer of genes and gene fragments in Staphylococcus extends beyond mobile elements". Journal of Bacteriology. 193 (15): 3964–77. doi:10.1128/JB.01524-10. PMC 3147504. PMID 21622749.
^ Kumarasamy KK, Toleman MA, Walsh TR, Bagaria J, Butt F, Balakrishnan R, et al. (September 2010). "Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study". The Lancet. Infectious Diseases. 10 (9): 597–602. doi:10.1016/S1473-3099(10)70143-2. PMC 2933358. PMID 20705517.
^ Hudson CM, Bent ZW, Meagher RJ, Williams KP (7 June 2014). "Resistance determinants and mobile genetic elements of an NDM-1-encoding Klebsiella pneumoniae strain". PLOS One. 9 (6): e99209. doi:10.1371/journal.pone.0099209. PMC 4048246. PMID 24905728.
^ Lou Z, Sun Y, Rao Z (February 2014). "Current progress in antiviral strategies". Trends in Pharmacological Sciences. 35 (2): 86–102. doi:10.1016/j.tips.2013.11.006. PMID 24439476.
^ Pennings PS (June 2013). "HIV Drug Resistance: Problems and Perspectives". Infectious Disease Reports. 5 (Suppl 1): e5. doi:10.4081/idr.2013.s1.e5. PMC 3892620. PMID 24470969.
^ Ton Q, Frenkel L (March 2013). "HIV drug resistance in mothers and infants following use of antiretrovirals to prevent mother-to-child transmission". Current HIV Research. 11 (2): 126–36. doi:10.2174/1570162x11311020005. PMID 23432488.
^ Ebrahim O, Mazanderani AH (June 2013). "Recent developments in hiv treatment and their dissemination in poor countries". Infectious Disease Reports. 5 (Suppl 1): e2. doi:10.4081/idr.2013.s1.e2. PMC 3892621. PMID 24470966.
^ Xie JL, Polvi EJ, Shekhar-Guturja T, Cowen LE (2014). "Elucidating drug resistance in human fungal pathogens". Future Microbiology. 9 (4): 523–42. doi:10.2217/fmb.14.18. PMID 24810351.
^ Srinivasan A, Lopez-Ribot JL, Ramasubramanian AK (March 2014). "Overcoming antifungal resistance". Drug Discovery Today: Technologies. 11: 65–71. doi:10.1016/j.ddtec.2014.02.005. PMC 4031462. PMID 24847655.
^ Costa C, Dias PJ, Sá-Correia I, Teixeira MC (2014). "MFS multidrug transporters in pathogenic fungi: do they have real clinical impact?". Frontiers in Physiology. 5: 197. doi:10.3389/fphys.2014.00197. PMC 4035561. PMID 24904431.
^ ab Andrews KT, Fisher G, Skinner-Adams TS (August 2014). "Drug repurposing and human parasitic protozoan diseases". International Journal for Parasitology. Drugs and Drug Resistance. 4 (2): 95–111. doi:10.1016/j.ijpddr.2014.02.002. PMC 4095053. PMID 25057459.
^ Visser BJ, van Vugt M, Grobusch MP (October 2014). "Malaria: an update on current chemotherapy". Expert Opinion on Pharmacotherapy. 15 (15): 2219–54. doi:10.1517/14656566.2014.944499. PMID 25110058.
^ Chia WN, Goh YS, Rénia L (2014). "Novel approaches to identify protective malaria vaccine candidates". Frontiers in Microbiology. 5: 586. doi:10.3389/fmicb.2014.00586. PMC 4233905. PMID 25452745.
^ Franco JR, Simarro PP, Diarra A, Jannin JG (2014). "Epidemiology of human African trypanosomiasis". Clinical Epidemiology. 6: 257–75. doi:10.2147/CLEP.S39728. PMC 4130665. PMID 25125985.
^ Herrera L (2014). "Trypanosoma cruzi, the Causal Agent of Chagas Disease: Boundaries between Wild and Domestic Cycles in Venezuela". Frontiers in Public Health. 2: 259. doi:10.3389/fpubh.2014.00259. PMC 4246568. PMID 25506587.
^ Mansueto P, Seidita A, Vitale G, Cascio A (2014). "Leishmaniasis in travelers: a literature review" (PDF). Travel Medicine and Infectious Disease. 12 (6 Pt A): 563–81. doi:10.1016/j.tmaid.2014.09.007. hdl:10447/101959. PMID 25287721.
^ Adedeji WA (December 2016). "THE TREASURE CALLED ANTIBIOTICS". Annals of Ibadan Postgraduate Medicine. 14 (2): 56–57. PMC 5354621. PMID 28337088.
^ Aminov RI (2010). "A brief history of the antibiotic era: lessons learned and challenges for the future". Frontiers in Microbiology. 1: 134. doi:10.3389/fmicb.2010.00134. PMC 3109405. PMID 21687759.
^ ab Organization, World Health (2014). Antimicrobial resistance : global report on surveillance. World Health Organization,. Geneva, Switzerland. ISBN 9789241564748. OCLC 880847527.
^ Amábile-Cuevas CF, editor. Antimicrobial resistance in bacteria. Horizon Scientific Press; 2007
^ Fleming A (11 December 1945). "Nobel Price Lecture" (PDF). nobelprize.org. Archived (PDF) from the original on 31 March 2018. Retrieved 1 March 2018.
^ "WHO | Global action plan on antimicrobial resistance". WHO. Archived from the original on 18 April 2018. Retrieved 23 April 2018.
^ President’s 2016 Budget Proposes Historic Investment to Combat Antibiotic-Resistant Bacteria to Protect Public Health Archived 11 March 2015 at the Wayback Machine. The White House, Office of the Press Secretary, January 27, 2015
^ ab Pollack A (20 January 2016). "To Fight 'Superbugs,' Drug Makers Call for Incentives to Develop Antibiotics". Davos 2016 Special Report. Davos, Switzerland: New York Times. Archived from the original on 24 April 2018. Retrieved 24 January 2016.
^ ab Behdinan A, Hoffman SJ (2015). "Some Global Strategies for Antibiotic Resistance Require Legally Binding and Enforceable Commitments". Journal of Law, Medicine & Ethics. 43 (2).
^ Hoffman SJ, Ottersen T (2015). "What Will It take to Address the Global Threat of Antibiotic Resistance?". Journal of Law, Medicine & Ethics. 43 (2): 363–368.
^ Rizvi Z, Hoffman SJ (2015). "Effective Global Action on Antibiotic Resistance Calls for Careful Consideration of the Convening Forum". Journal of Law, Medicine & Ethics. 43 (2).
^ Andresen S, Hoffman SJ (2015). "Much Can Be Learned about Addressing Antibiotic Resistance from Multilateral Environmental Agreements". Journal of Law, Medicine & Ethics. 43 (2): 46–52.
^ ab "FACT SHEET: Obama Administration Releases National Action Plan to Combat Antibiotic-Resistant Bacteria". whitehouse.gov. Archived from the original on 22 November 2015. Retrieved 30 October 2015.
^ Doan Q, Enarson P, Kissoon N, Klassen TP, Johnson DW (September 2014). "Rapid viral diagnosis for acute febrile respiratory illness in children in the Emergency Department". The Cochrane Database of Systematic Reviews. 9 (9): CD006452. doi:10.1002/14651858.CD006452.pub4. PMID 25222468.
^ Mishra RP, Oviedo-Orta E, Prachi P, Rappuoli R, Bagnoli F (October 2012). "Vaccines and antibiotic resistance". Current Opinion in Microbiology. 15 (5): 596–602. doi:10.1016/j.mib.2012.08.002. PMID 22981392.
^ "Immunity, Infectious Diseases, and Pandemics—What You Can Do". HomesteadSchools.com. Archived from the original on 3 December 2013. Retrieved 12 June 2013.
^ Kim S, Lieberman TD, Kishony R (October 2014). "Alternating antibiotic treatments constrain evolutionary paths to multidrug resistance". Proceedings of the National Academy of Sciences of the United States of America. 111 (40): 14494–9. Bibcode:2014PNAS..11114494K. doi:10.1073/pnas.1409800111. PMC 4210010. PMID 25246554.
^ Pál C, Papp B, Lázár V (July 2015). "Collateral sensitivity of antibiotic-resistant microbes". Trends in Microbiology. 23 (7): 401–7. doi:10.1016/j.tim.2015.02.009. PMC 5958998. PMID 25818802.
^ Imamovic L, Sommer MO (September 2013). "Use of collateral sensitivity networks to design drug cycling protocols that avoid resistance development". Science Translational Medicine. 5 (204): 204ra132. doi:10.1126/scitranslmed.3006609. PMID 24068739. Archived from the original on 5 February 2018. Retrieved 4 February 2018.
^ Imamovic L, Ellabaan MM, Dantas Machado AM, Citterio L, Wulff T, Molin S, Krogh Johansen H, Sommer MO (January 2018). "Drug-Driven Phenotypic Convergence Supports Rational Treatment Strategies of Chronic Infections". Cell. 172 (1–2): 121–134.e14. doi:10.1016/j.cell.2017.12.012. PMC 5766827. PMID 29307490. Archived from the original on 9 January 2018. Retrieved 4 February 2018.
^ Liu J, Bedell TA, West JG, Sorensen EJ (June 2016). "Design and Synthesis of Molecular Scaffolds with Anti-infective Activity". Tetrahedron. 72 (25): 3579–3592. doi:10.1016/j.tet.2016.01.044. PMC 4894353. PMID 27284210.
^ "Annual Report of the Chief Medical Officer - Infections and the rise of antimicrobial resistance" (PDF). UK NHS. 2011. Archived from the original (PDF) on 30 October 2013.
^ ab "Obama Administration Seeks To Ease Approvals For Antibiotics". NPR. 4 June 2013. Archived from the original on 13 March 2015. Retrieved 7 August 2016.
^ "Moldova Grapples With Whether To Isolate TB Patients". NPR. 4 June 2013. Archived from the original on 3 August 2016. Retrieved 7 August 2016.
^ ab Walsh F. "BBC News — Antibiotics resistance 'as big a risk as terrorism' – medical chief". Bbc.co.uk. Archived from the original on 8 August 2018. Retrieved 12 March 2013.
^ Khor M (18 May 2014). "Why Are Antibiotics Becoming Useless All Over the World?". The Real News. Archived from the original on 18 May 2014. Retrieved 18 May 2014.
^ Nordrum A (2015). "Antibiotic Resistance: Why Aren't Drug Companies Developing New Medicines to Stop Superbugs?". International Business Times.
^ Gever J (4 February 2011). "Pfizer Moves May Dim Prospect for New Antibiotics". MedPage Today. Archived from the original on 14 December 2013. Retrieved 12 March 2013.
^ Ledford H (December 2012). "FDA under pressure to relax drug rules". Nature. 492 (7427): 19. Bibcode:2012Natur.492...19L. doi:10.1038/492019a. PMID 23222585.
^ Press Release (12 December 2013). "Green, Gingrey Introduce ADAPT Act to Safeguard Public Health". U.S. Congress. Archived from the original on 20 December 2013. Retrieved 19 December 2013.
^ "Antibiotic Development to Advance Patient Treatment Act of 2013" (PDF). U.S. Congress. 12 December 2013. Archived (PDF) from the original on 3 March 2016. Retrieved 19 December 2013.
^ Office of the Press Secretary (18 September 2014). "Executive Order – Combating Antibiotics-Resistant Bacteria". The White House. Archived from the original on 22 September 2014. Retrieved 22 September 2014.
^ President's Council of Advisors on Science and Technology (September 2014). "Report to the President on Combating Antibiotic Resistance" (PDF). PCAST. Archived (PDF) from the original on 22 September 2014. Retrieved 22 September 2014.
^ "Diagnostics Are Helping Counter Antimicrobial Resistance, But More Work Is Needed". MDDI Online. 2018-11-20. Retrieved 2018-12-02.
^ ab van Belkum A, Bachmann TT, Lüdke G, Lisby JG, Kahlmeter G, Mohess A, Becker K, Hays JP, Woodford N, Mitsakakis K, Moran-Gilad J, Vila J, Peter H, Rex JH, Dunne WM (January 2019). "Developmental roadmap for antimicrobial susceptibility testing systems". Nature Reviews. Microbiology. 17 (1): 51–62. doi:10.1038/s41579-018-0098-9. PMID 30333569.
^ "Progress on antibiotic resistance". Nature. 562 (7727): 307. October 2018. doi:10.1038/d41586-018-07031-7. PMID 30333595.
^ "Silent Killers: Fantastic Phages?". Archived from the original on 10 February 2013. Retrieved 14 November 2017.
^ McAuliffe, et al. (2007). "The New Phage Biology: From Genomics to Applications" (introduction)". In McGrath S, van Sinderen D. Bacteriophage: Genetics and Molecular Biology. Caister Academic Press. ISBN 978-1-904455-14-1.CS1 maint: Explicit use of et al. (link)
^ ab Lin DM, Koskella B, Lin HC (August 2017). "Phage therapy: An alternative to antibiotics in the age of multi-drug resistance". World Journal of Gastrointestinal Pharmacology and Therapeutics. 8 (3): 162–173. doi:10.4292/wjgpt.v8.i3.162. PMC 5547374. PMID 28828194. Archived from the original on 24 April 2018. Retrieved 23 April 2018.
^ ab Salmond GP, Fineran PC (December 2015). "A century of the phage: past, present and future". Nature Reviews. Microbiology. 13 (12): 777–86. doi:10.1038/nrmicro3564. PMID 26548913.
^ Letarov AV, Golomidova AK, Tarasyan KK (April 2010). "Ecological basis for rational phage therapy". Acta Naturae. 2 (1): 60–72. PMC 3347537. PMID 22649629.
^ Parfitt T (June 2005). "Georgia: an unlikely stronghold for bacteriophage therapy". Lancet. 365 (9478): 2166–7. doi:10.1016/S0140-6736(05)66759-1. PMID 15986542.
^ Golkar Z, Bagasra O, Pace DG (February 2014). "Bacteriophage therapy: a potential solution for the antibiotic resistance crisis". Journal of Infection in Developing Countries. 8 (2): 129–36. doi:10.3855/jidc.3573. PMID 24518621.
^ McCallin S, Alam Sarker S, Barretto C, Sultana S, Berger B, Huq S, Krause L, Bibiloni R, Schmitt B, Reuteler G, Brüssow H (September 2013). "Safety analysis of a Russian phage cocktail: from metagenomic analysis to oral application in healthy human subjects". Virology. 443 (2): 187–96. doi:10.1016/j.virol.2013.05.022. PMID 23755967.
^ Abedon ST, Kuhl SJ, Blasdel BG, Kutter EM (March 2011). "Phage treatment of human infections". Bacteriophage. 1 (2): 66–85. doi:10.4161/bact.1.2.15845. PMC 3278644. PMID 22334863.
Books
.mw-parser-output .refbegin{font-size:90%;margin-bottom:0.5em}.mw-parser-output .refbegin-hanging-indents>ul{list-style-type:none;margin-left:0}.mw-parser-output .refbegin-hanging-indents>ul>li,.mw-parser-output .refbegin-hanging-indents>dl>dd{margin-left:0;padding-left:3.2em;text-indent:-3.2em;list-style:none}.mw-parser-output .refbegin-100{font-size:100%}
Caldwell R, Lindberg D, eds. (2011). "Understanding Evolution" [Mutations are random]. University of California Museum of Paleontology.
Reynolds LA; Tansey EM, eds. (2008). Superbugs and superdrugs : a history of MRSA : the transcript of a Witness Seminar held by the Wellcome Trust Centre for the History of Medicine at UCL, London, on 11 July 2006. London: Wellcome Trust Centre for the History of Medicine at UCL. ISBN 978-0-85484-114-1.
Journals
Anomaly J (2017). Antibiotics and Public Policy (PDF). Georgetown University Press.
Arias CA, Murray BE (January 2009). "Antibiotic-resistant bugs in the 21st century--a clinical super-challenge". The New England Journal of Medicine. 360 (5): 439–43. doi:10.1056/NEJMp0804651. PMID 19179312.
Goossens H, Ferech M, Vander Stichele R, Elseviers M (2005). Esac Project. "Outpatient antibiotic use in Europe and association with resistance: a cross-national database study". Lancet. Group Esac Project. 365 (9459): 579–87. doi:10.1016/S0140-6736(05)17907-0. PMID 15708101.
Hawkey PM, Jones AM (September 2009). "The changing epidemiology of resistance" (PDF). The Journal of Antimicrobial Chemotherapy. 64 Suppl 1: i3–10. doi:10.1093/jac/dkp256. PMID 19675017.
Soulsby EJ (November 2005). "Resistance to antimicrobials in humans and animals". BMJ. 331 (7527): 1219–20. doi:10.1136/bmj.331.7527.1219. PMC 1289307. PMID 16308360.
"Alternatives to Antibiotics Reduce Animal Disease". Commonwealth Scientific and Industrial Research Organization. 9 Jan 2006.
Cooke P, Rees-Roberts D (2017). CATCH. 16-minute film about a post-antibiotic world. Review: Sansom C (March 2017). "Media Watch: An intimate family story in a world without antibiotics". Lancet Infect Dis. 17 (3): 274. doi:10.1016/S1473-3099(17)30067-1.
External links
| Wikimedia Commons has media related to Antibiotic resistance. |
Wikipedia's health care articles can be viewed offline with the Medical Wikipedia app.
Antimicrobial resistance at Curlie
- Animation of Antibiotic Resistance
- CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
Antimicrobial Stewardship Project, at the Center for Infectious Disease Research and Policy (CIDRAP), University of Minnesota
AMR Industry Alliance, "members from large R&D pharma, generic manufacturers, biotech, and diagnostic companies"

Comments
Post a Comment